How Many Eggs Does A Woman Have?
Women are born with a finite number of eggs. At birth, the ovaries contain anywhere from one million to two million eggs. At the start of puberty, this has decreased to 300,000 to 400,000 eggs. By the age of 40, the average number of eggs remaining stands at 5,000 to 10,000. This article answers common questions about egg numbers, ovulation and age. We cover the number of eggs women have at different life stages, how many eggs are released per cycle and how age and lifestyle factors affect egg quality.

Questions about women's eggs and fertility
- How many eggs does a woman have?
- How many eggs does a woman have at every age?
- Are women born with all their eggs?
- How many eggs do women have during their lifetime?
- How many eggs does a woman produce each month?
- How many eggs are released during ovulation?
- How do I know how many eggs I have right now?
- Does the quality of the eggs decrease with age?
- Can you improve egg quality?
- Are egg quality and quantity related?
- What are the signs of low egg count?
- Can you get pregnant with low eggs?
- What do human eggs look like?
- What happens to all the lost eggs?
How many eggs does a woman have?
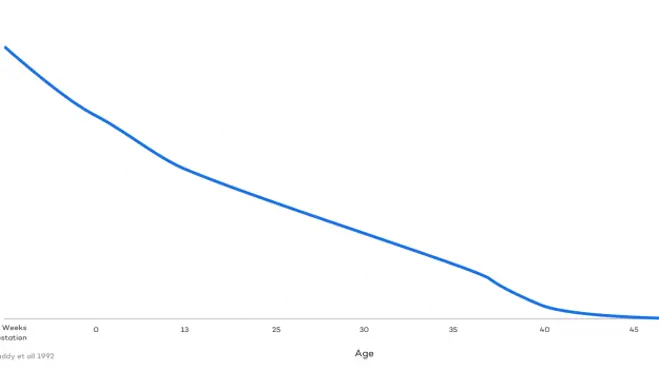
A woman has a fixed number of eggs, and that egg count decreases throughout life. The ovaries contain around seven million eggs during female foetal development. At birth, this figure has dropped to around one million to two million eggs. By puberty, 300,000 to 400,000 eggs remain, and at 30 years of age, the ovarian reserve has 100,000 to 150,000 eggs.
The term ovarian reserve means the number of eggs remaining in the ovaries. A lower ovarian reserve and age-related changes in egg quality can reduce the likelihood of conception over time.
The reduction in the quantity and quality of the eggs affects fertility and decreases the likelihood of conception as a woman ages. This does not mean that older women cannot conceive without fertility treatment. But it may take longer to do so. When the woman is under 40, eight in ten couples will conceive without fertility treatment within 12 months if they are having regular unprotected sex during the fertility window (NHS).
How many eggs does a woman have at every age?
Are women born with all their eggs?
Women are born with all the eggs they will ever have. However, the egg reserve has already begun to decrease by the time of birth. Peak egg supply is typically reached at around 20 weeks of gestation, when the female ovaries contain approximately seven million eggs. At birth, this has decreased to somewhere between one and two million eggs.
How many eggs do women have during their lifetime?
Women start life with around 1 to 2 million eggs, and the total decreases over time. Therefore, women have a finite number of eggs. This figure gradually decreases as mature eggs are ovulated and immature eggs are broken down and reabsorbed by the body.
While every female body is different, that initial supply of eggs is typically exhausted by the age of 52. This is the average age at which the menopause begins.
How many eggs does a woman produce each month?
A woman typically produces one mature egg each month. By “produce”, we refer to the process where she matures and releases one egg per menstrual cycle.
Immature eggs are matured within small sacs of fluid called follicles. One follicle grows one egg. Follicles are recruited and stimulated throughout the menstrual cycle and take around 90 days to reach the point at which they can release a mature egg. The body stimulates a large number of follicles at once to maximise the chances that the strongest egg is the one ovulated.
Research suggests that 30 to 40 follicles are stimulated and leave the ovarian reserve every day. At any one moment, somewhere between 500 and 1,000 eggs are in the process of being developed.
How many eggs are released during ovulation?
One mature egg is released during ovulation. This means that there is usually only one egg for sperm to fertilise every menstrual cycle. If this egg is not fertilised, it begins to break down and is released in a woman’s period.
Follicles that are not dominant and do not release the mature egg die off, are broken down and reabsorbed by the body, along with the immature eggs. This happens to around 1,000 follicles every month.
How do I know how many eggs I have right now?
Fertility specialists can estimate how many eggs remain in your ovarian reserve using the anti-Müllerian hormone (AMH) test or a transvaginal ultrasound scan.
- Anti-Müllerian hormone (AMH) test: AMH is produced in the ovarian follicles, and measuring it enables specialists to estimate how many eggs remain. Higher AMH measurements indicate a larger number of eggs. The test is also used to assess how well the ovaries might respond to certain fertility medications.
- Transvaginal ultrasound: This scan is known as an Antal Follicle Count, this test counts the visible follicles in the ovaries. As each follicle contains an immature egg, this allows for a good estimation of the number of eggs remaining.
It is important to note that both tests only estimate the number of eggs remaining in the reserve and do not account for the quality of those eggs. In this instance, egg quality refers to the likelihood that an egg can lead to a healthy embryo.
Does the quality of the eggs decrease with age?
Yes, the quality of eggs does decrease with age. Research shows that, as women age, the likelihood of a genetically abnormal embryo increases. This reflects an age-related decline in egg quality. At the age of 30, there is a 24% chance of a genetically abnormal embryo. By the time a woman reaches 45, this has increased to an 84% chance (Franasiak et al.).
Can you improve egg quality?
There is little scientific evidence to suggest that we can improve egg quality through medications or lifestyle changes. Age is the most important factor associated with egg quality. Women in their 20s are likely to have a significantly higher percentage of healthy, genetically normal eggs than women in their 30s.
That said, some early studies suggest there may be ways to improve egg quality:
- Omega-3 fatty acids: a diet rich in omega-3 fatty acids may improve egg quality (Nehra et al.).
- Coenzyme Q10: also known as CoQ10, this antioxidant may improve egg quality (Jiang et al.).
- Quit smoking: the chemicals in cigarettes have been shown to reduce egg quantity and quality, as well as impair ovarian functions. Women who smoke typically experience menopause around one to four years earlier than those who do not smoke.
It is important to note that there is currently insufficient scientific evidence to definitively connect either omega-3 fatty acids or CoQ10 with improved egg quality. More research is required to establish a causal relationship.
Though there are no proven ways to improve egg quality, you can improve overall health and the likelihood of successful conception in the following ways:
- Reduce exposure to stress.
- Eat a nutrient-rich diet.
- Participate in regular exercise.
- Avoid toxins, such as pesticides and heavy metals.
What are the signs of low egg count?
There are no symptoms or signs of a low egg count in most cases. Typically, the only sign of a low egg count is difficulty conceiving and becoming pregnant. In some instances, a low egg count may result in:
- Shortened menstrual cycles.
- Heavier periods.
- Absent periods.
- Hot flushes.
However, all of these symptoms are also associated with other reproductive and fertility issues, and don’t necessarily indicate a low egg count. The only way to get a reasonably accurate estimate of your egg count is with a transvaginal ultrasound or the AMH test.
Can you get pregnant with low eggs?
Yes, you can get pregnant with a lower egg count, and many people do. You only need one viable egg for fertilisation to occur, and this can happen as long as the body is still capable of maturing eggs. However, your chances of successfully conceiving are reduced with a lower egg count.
You can significantly increase the likelihood of pregnancy with fertility treatments like IVF (in vitro fertilisation). Many women with a lower egg count may also consider using a donor egg or freezing healthy eggs for the future. European Sperm Bank can guide you on the path with useful information about donor eggs and support options for people exploring this route. We can help you find an egg donor.
What do human eggs look like?
Healthy human eggs are spherical and about the size of a grain of sand. They measure approximately 100 micrometres (µm) in diameter and are the largest cells in the human body.
Despite their size, you’ll typically need a microscope to see them, under which they will appear slightly yellowish or off-white with a clear nucleus. They are surrounded by a clear cytoplasm that provides the cell with many of the nutrients it needs.
Unhealthy eggs may be an irregular shape, appear darker than healthy egg cells or have a granular cytoplasm.

What happens to all the lost eggs?
Mature eggs that are not fertilised are broken down and released with a woman’s menstrual fluid. Immature eggs that were developed but not selected as the dominant egg are broken down and absorbed by the body.
Next steps on your path to parenthood
At European Sperm Bank, we aim to help aspiring parents make an informed choice about fertility treatments and the path to parenthood. If you’re looking to take the next steps on your journey, our guides are the perfect place to find more information.

